How Myanmar achieved the 2020 milestone of reducing TB disease burden
27 February 2023
Myanmar is the only country in the Region to achieve the 2020 deadline for the SDG target of 20% reduction of TB incidence from the 2015 baseline.
Collaboration of the public and private sectors has played an important role in the efforts to control TB.
An increase in government spending on TB, newer diagnostic tools, use of mobile clinics, and making treatment affordable are some of the key elements of Myanmar’s approach to combat TB.
Every year more than 10 million people fall ill from tuberculosis (TB), a bacterial infection that mainly affects the lungs. Despite being preventable and curable, TB disease claims 1.5 million lives globally every year.
Most of those who fall ill with TB live in low and middle-income countries. The World Health Organization’s South-East Asia Region, home to 26% of the world’s population, has 43% of the global TB burden.
Eliminating tuberculosis was declared a Regional Flagship Priority Programme in 2017 by Dr Poonam Khetrapal Singh, Regional Director of WHO South-East Asia Region. WHO SEARO continues to provide policy, strategic and operational technical support to the national TB programmes and to partners in its Member States.
Myanmar is one of the countries with a high burden of TB, TB-HIV and drug-resistant TB. As per the Global Tuberculosis Report 2021 of WHO, an estimated 167000 people fell ill with TB in the country. An estimated 22000 deaths occurred in the country due to the disease, including 2900 deaths of people living with HIV, in 2020.
There were also an estimated 10000 new cases of rifampicin-resistant (RR) and multidrug-resistant (MDR) TB emerging in the year. The biggest social determinants and drivers of TB in Myanmar are undernourishment (40000), smoking (19000), HIV (14000), alcohol use (7700) and diabetes (6500).
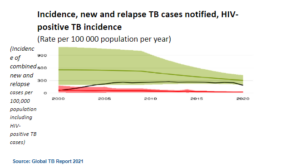
While all countries in the Region have continued to accelerate efforts to end TB, Myanmar is among a few high-TB burden countries and the only one in the WHO SE Asia Region to achieve the 2020 milestone targets of a 20% reduction of TB incidence from the 2015 baseline, in alignment with the WHO End TB Strategy which is in turn aligned with the United Nations’ Sustainable Development Goals related to ending TB by 2030.
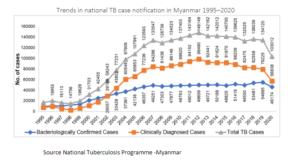
Myanmar has been battling TB since 1966. However, it was during 2009–2010 that the real extent of the TB burden in Myanmar began to emerge. The National TB Prevalence Survey was concluded by the National Tuberculosis Programme in April 2010 and revealed that the prevalence of TB was three times higher than previously thought while incidence was more than double.
The data generated through the prevalence surveys and national TB surveillance system was carefully analysed and the information shared with national and international experts. In addition, joint monitoring missions (JMM) were held to understand progress, strengths, weaknesses and the way forward. Based on this, a National Strategic Plan was developed through a consultative process that included TB experts, public health experts, service providers, the private sector, people affected with the disease, and the like.
Subsequently, in 2011 the Myanmar Health Sector Coordination Committee (M-HSCC) was formed. It provides technical support across various pillars of the TB programme, including support in developing the Global Fund proposal and programme planning, implementation and monitoring. This partnership acted as a catalyst for the NTP on timely and quality action.
Myanmar’s key interventions in the campaign against TB with the private sector
Since 2000, WHO has been encouraging public-private partnership projects to control TB globally. In 2003, the Ministry of Health and Sports, Myanmar developed guidelines to involve private general practitioners (GPs) in the National Tuberculosis Programme (NTP).

The expansion of TB care in a public–private mix (PPM) or as a collaboration of the public and private sector has played an important role in Myanmar’s campaign to control TB by increasing case finding and quality of care. The PPM contributed to 25% of the total case notification in 2020.
By the end of 2018, a total of 2965 GPs were involved in PPM TB activities. The treatment success rate for all forms of TB treated by GPs was 88% in 2017 cohort. Good and timely planning enabled the expansion and strengthening of TB service coverage (particularly in the states) and improved links with the private sector.
Drug shops or pharmacies located in communities are often the first points of contact for people seeking health care. As part of the TB control programme drug shops or pharmacies were roped in to screen presumptive TB cases and make referrals to public health clinics. In 2011, with the support of the TB-Reach Wave 2 Fund, Population Services International accelerated TB case-finding activity (ACF or Active Case Finding)through Myanmar’s drug seller-initiated programme. In 2012, the Japan International Cooperation Agency (JICA) piloted the model of accelerated TB case-finding by pharmacies in three townships and PSI adopted the model and scaled it up to 70 townships in 2017.
A total of 51 259 cases were referred by drug sellers (during 2015–2018) and 12 404 (24%) cases were diagnosed as TB from among those referrals.
Community-based TB care (CBTBC) services are another important activity that supported the accelerated diagnosis of cases through increased community awareness about TB. This includes screening people for TB, referring presumptive TB cases for confirmation of diagnosis, supporting sputum collection and transport, and providing home-based DOT to patients. From 1% in 2011, CBTBC notifications of all forms of TB reached 12.9% in 2019.
Mobile clinic operations was another important component of the NTP programme in Myanmar. Through WHO technical support, NTP developed standard operating procedures for mobile teams and provided training to all team members consisting of team leaders, medical officers, radiographers, X-ray assistants, laboratory technicians and data assistants.
Additional human resources were contributed by local and international NGOs. From 2011 to 2017, a total of 21 115 TB cases were identified and could be treated using mobile clinics. In 2018, 439 mobile team visits were conducted; including at urban sites, areas considered hard to reach, prisons and their worksites, industrial sites and camps of internally displaced persons (IDP).
Similarly, the NTP also collaborated with the Ministry of Health and Ministry of Home Affairs for the screening of TB cases in a few prisons in Myanmar. Since 2016, entry screening for TB and HIV has also been conducted in Insein and Mandalay central prison.
Newer tools and ease of diagnosis
In order to bring quality screening and diagnostic services closer to the community, a network of laboratories was set up and expanded from 417 in 2011 to 516 in 2019. The expansion of these services also made it possible to treat patients who may not remain in the community with their disease for too long and move to another area.
Following the inception of fluorescence microscopy (FM) in 2012, 25 units were introduced in microscopy centres located in high-workload areas, and 149 added in 2014. The phase-in process continued till 2019. All the township TB centres have been using FM microscopy which has higher sensitivity than traditional bright-field microscopes with ZN (Ziehl-Neelsen) stain, thereby increasing TB case detection. ZN stain is a rapid and practical method for detecting acid-fast bacilli (AFB), especially in low-income countries, due to its rapidity, low cost, and high positive predictive value for tuberculosis.

A session held to install multidrug-resistant tuberculosis software and machinery (Photo credit: WHO Myanmar)
Making treatment affordable
According to the Global Health Expenditure Database (WHO), in the last five years, the health expenditure per capita increased 2.7 times from US$ 23.28 in 2012 to US$ 62.11 in 2016. Out-of-pocket expenditure as per the catastrophic cost survey has also increased from 69.26% in 2012 to 73.98% in 2016.
MoHP policy has enabled all other essential drugs to be available free of charge to patients through public facilities. This has helped reduce out-of-pocket payments. People are using public health services more than they did before.
Prevention and reduction of TB transmission is faster when both diagnosis and treatment are free of charge. This policy was the same in both the public sector as well as the private sector. As more people are using public health services than before, this stands to benefit TB care. Frontline health workers continue to be alert about identifying presumptive cases among patients where all required diagnostics are not available.
TB funding and government spending on TB control has also increased annually from 2014. The government’s financial support is mainly with first- and second-line anti-TB drugs, infrastructure and human resources. Since 2017, the MoH has been procuring 100% of first-line TB drugs used in the country and 40% of second-line TB drugs, and has also instituted an effective procurement and distribution system for TB drugs. Notably, no stock-outs of drugs were observed nor were reported by the joint monitoring mission (JMM).
Major funding support has also been provided by the Global Fund, the 3 Diseases Fund, the MDG Fund, Access to Health Fund, USAID and WHO to bridge the key gaps in TB programme financing. For the implementation of National TB Strategic Plan 2015–2020, domestic funding of US$ 1.8 million was mobilized, and complemented by international donor funding of US$ 37 million. Such investments have allowed improved access to quality TB care throughout the country. Capacity-building and accelerated case finding (ACF) could be supported to detect cases early and bring them under treatment.
Challenges and the road ahead
One of the main challenges in Myanmar is the presence of a very large number of people who survived TB without treatment. Moreover, high transmission of TB in congested urban areas in the country has also been suggested in surveys.
TB prevalence continues to exceed 600/100 000 population, the HIV-TB co-infection rates hover at 13%. Smoking damages the lungs and smokers are more susceptible to TB infection; 25% of men and 7% of women in the country smoke.
The COVID-19 pandemic has also severely impacted progress in eliminating TB in Myanmar. The case notification of all forms of TB in 2020 decreased by 20% compared with 2019. DR-TB notification and childhood TB notification decreased by 80% during the same time frame. Following the political situation after 1 February 2021, public health facilities were largely non-functional for about six months. As a result, the total number of cases notified in 2021 dropped further, data for which is yet to be released.
Due to the TB service disruptions, TB diagnosis by chest X-ray examination has been stopped temporarily in a few areas that show high levels of COVID-19 community transmission. Limited TB diagnosis is undertaken due to the civil disobedience movement, and there has been a decline in referrals of presumptive TB cases by community volunteers and temporary interruption of mobile team activities. Multisectoral response and coordination across ministries is inadequate and will be needed to sustain the gains made so far and accelerate progress to combat TB.
Another area of concern for TB diagnosis services is the understaffing in the public health sector. This is particularly true about the availability of specialized personnel such as microbiologists, laboratory technicians, biomedical engineers, radiographers and X-ray technicians, and staff for administrative work including infection control. The increasing workload in the wake of human resource limitation has been an important challenge. TB care cannot be halted and efforts to resume care are being rewarded as several facilities that were earlier shut have resumed offering services.
Overcoming challenges
These challenges can be overcome by finding the cases that missed detection during the beginning of the pandemic and due to the ongoing political situation. For this to happen, resumption of operations of the public sector needs to be a priority. Partner agencies need to also step up their support until access to public health facilities becomes optimal.
 A review meeting with community health volunteers to discuss measures to spread awareness about tuberculosis in November 2021 in Myanmar (Photo credit: WHO-Myanmar)
A review meeting with community health volunteers to discuss measures to spread awareness about tuberculosis in November 2021 in Myanmar (Photo credit: WHO-Myanmar)
Active case detection, focusing existing resources on high TB-burden sites, and strengthening public health systems in areas where the political situation is stable can be the starting point. Integrated testing for TB and COVID-19 has been initiated and is helping to find some of the missing TB cases.
All oral MDR-TB (multidrug-resistant TB) regimens will be scaled up throughout the country and a shorter treatment drug regimen for drug-sensitive TB, which is already approved and recommended by WHO, will be promoted. Introduction of new tools including molecular diagnostics of TB that are capable of testing susceptibility to anti-TB drugs has begun and will be scaled up. Additional new innovations to improve the accuracy of screening and TB diagnosis, compliance to treatment, and increased chances of treatment success are being promoted.
TB preventive treatment guidelines have been updated, public health workers have been trained to deliver TPT and the programme has plans to scale up the intervention throughout the country.
Yangon: a case study
The Yangon Region is the most populous region of Myanmar and constitutes 12% of the country’s population. However, drug-sensitive TB cases notified in that Region constituted 24–25% of the country’s caseload. A major concern is the drug-resistant TB caseload, which was 44%, and the TB/HIV burden, which was 30–35% of the national country caseload. Success in the Yangon Region will define success in TB control across the country.
Considering the crisis situation with TB in Yangon, a tailored approach was necessary. WHO supported the Yangon Health Department and NTP to develop a regional plan to tackle its specific challenges in urban and peri-urban areas. With this support ‘Yangon Consortium TB Project composed of CSOs and NGOs was formed to cope with urban and peri-urban issues. The targets of the consortium project were particularly vulnerable populations, including internal migrants and displaced populations, who had limited access to public services.
There is further scope to improve collaboration with the National AIDS Programme to address TB in Myanmar. In 2019, only 78% of HIV-positive people with new or relapsed TB incidence were started on antiretroviral therapy and 90% on chemo-prophylactic treatment. There is scope to further improve access to these drugs for all people diagnosed with TB. For further progress, the role of WHO is undeniably crucial.

